‘Which study should I read next?’ is a simple question but strikes the core of a radiology team’s workflow. Most practices implement a version of first-in-first-out queues grouped by a priority level (e.g. ER, Routine). Radiologists are generally expected to complete all urgent tasks prior to moving to lower priority studies.
The problem with treating studies first-in-first-out, or FIFO, is that lower priority studies can be continually ‘starved’ and miss deadlines (Mustafa and Talab, 2016). One of our goals at Inflo Health was to develop a better ranking that maximized the number of studies returned within their due date. We hypothesized that allowing for more flexibility would find time in a worklist for lower priority items without compromising emergent studies.
Borrowing from operations research
Non-preemptive priority queues have been well described in the operations research literature since the 1960’s. These advances already govern tasks that affect your daily life. For example, how your network packet is picked up by the router in the crowded public wifi.
One interesting algorithm from the operations research literature that can inform our question is shortest processing time, or SPT. If you have four jobs to complete, you can accomplish SPT by completing the easiest task first, then the next easiest, until your complete.
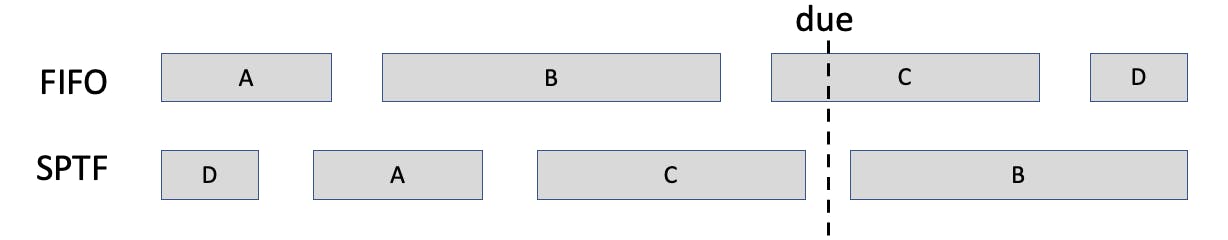
In this impossible example imagine you have four tasks all due at the time, but not enough time to finish them. If you prioritize the order they arrived (A-B-C-D) you only complete A and B before the deadline. If you focus on the easiest task first (D-A-C-B), then you can complete A, C, and D.
Application to Radiology
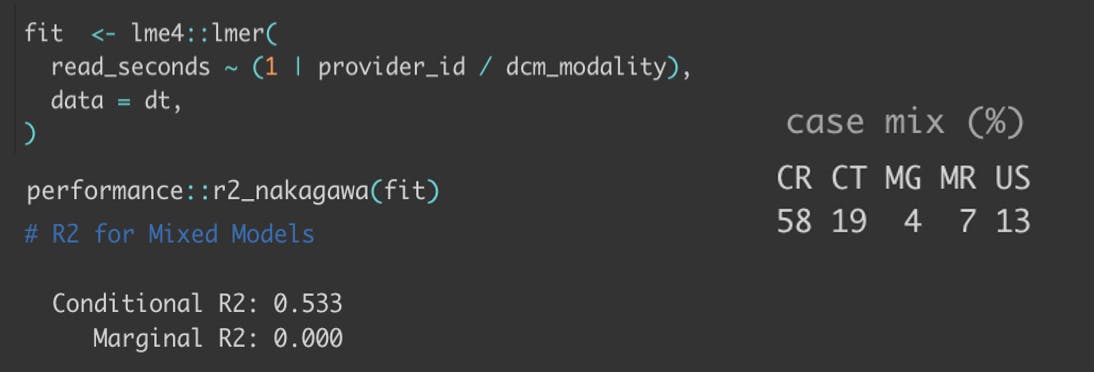
One important extension of this SPT heuristic is that is still useful in the context of incomplete information. The radiologist’s interpretation time of a given study is not known at the time of arrival, but that doesn’t mean it’s impossible to model. In our collaboration with a national teleradiology firm, we have found these times to be largely consistent across time. In fact, we can explain over half to the variation in interpretation times with a hierarchical linear model with only two intercepts — who are you, and which modality are you reading? This doesn’t take into account radiologist specialty, the priority a study was ordered under, or even anything specific about the imaging location!
Validation through simulation
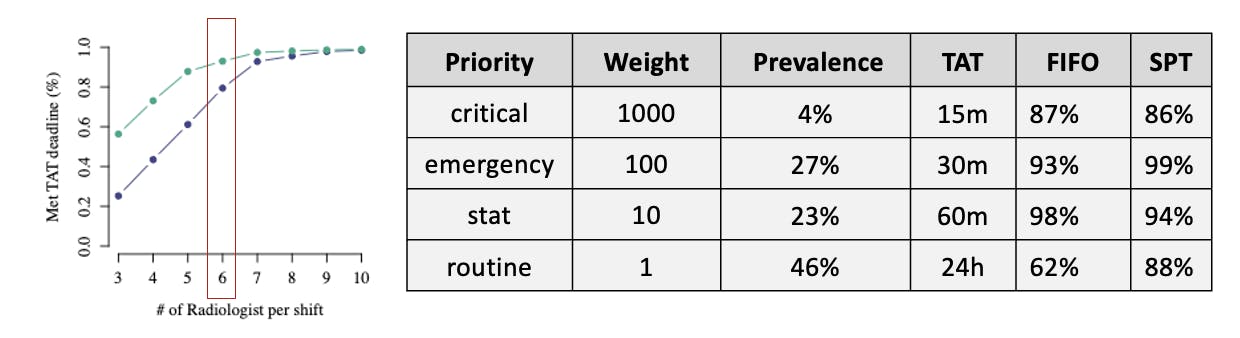
We utilized a simulation to prove out a different queue mechanism can improve study turnaround times without compromising emergent reads. In each replicate, we estimated what would have happened if a different prioritization strategy had been used given a fixed supply of radiologists. Each simulation was modeled at the level of a minute for thirty days. We parameterized each replicate with real studies drawn from a time series of two years from our partner teleradiology firm. Each replicate had a random starting point with study arrival times shuffled randomly.
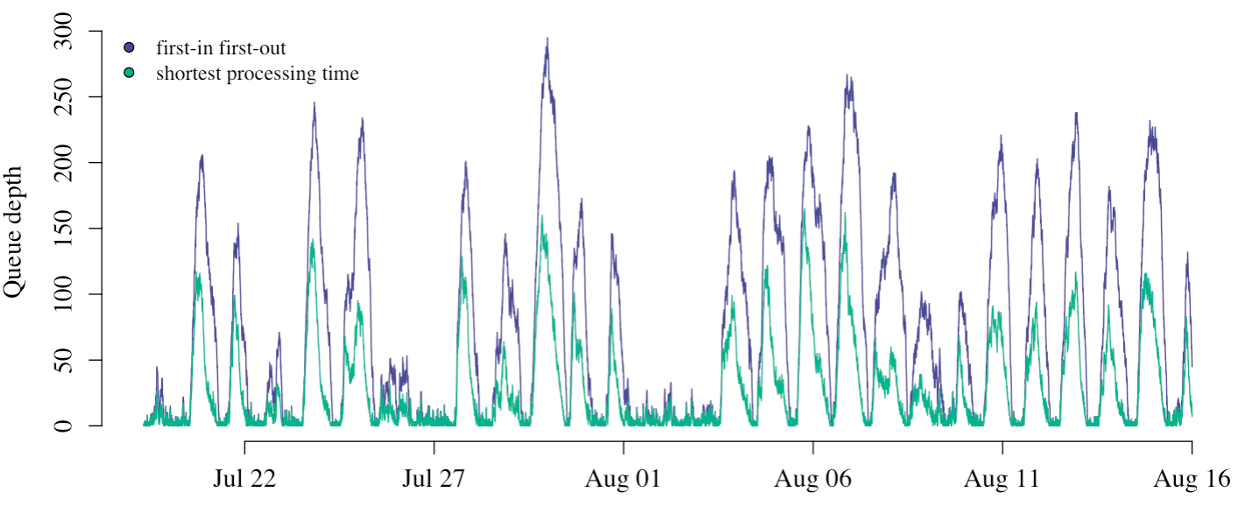
How many studies are in the worklist is a good proxy for overall team performance in each replicate.
We aggregate three key performance metrics to describe the radiology team’s performance in each replicate.
- What percentage of studies were completed on time? On average we saw a 13% increase in the completion percentage across radiologist budgets.
- How quickly were studies completed? Note the log10 scale, but it's no surprise studies were consistently returned faster with SPT prioritization.
- What percentage of studies were completed after business hours? On average we saw 11% fewer studies read after hours across radiologist budgets.
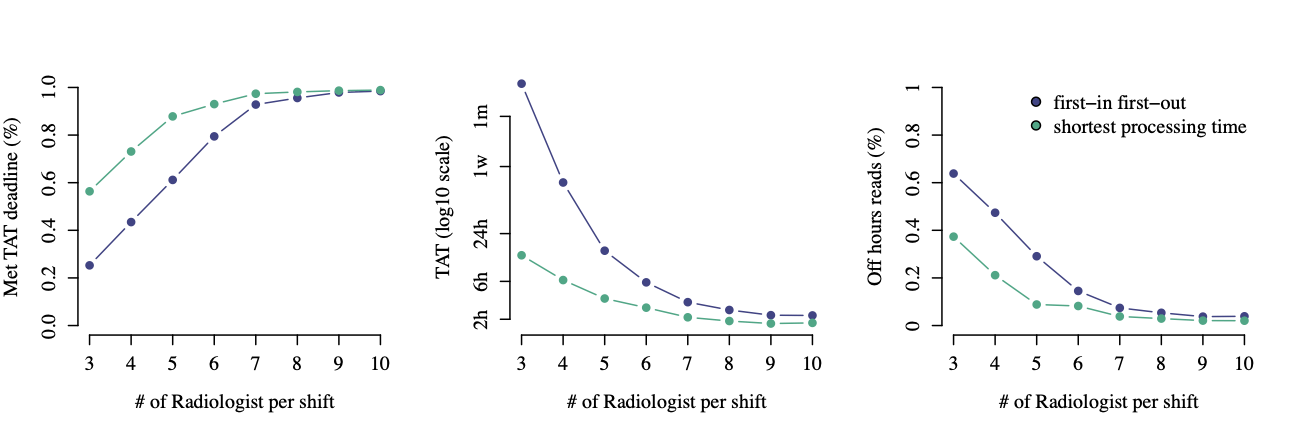
The benefits of SPT prioritization were higher in simulations with a more constrained supply of radiologists. It’s no surprise they converged in simulations with an excess supply.
We were able to maintain standards of care in different priority queues by weighting the processing time by a coefficient (e.g. weighted SPT). Let t represent the time it will take to read a study and w its priority weight. Weighted SPT is simply ordering a worklist by the ratio t / w.
Want to leverage what we've built?
We’ve built AI tools to help reduce turnaround times that plug into existing PACS/RIS platforms. We’ve seen that through AI-backed worklist management, we can improve turnaround times (TAT) in all study categories. Reach out to us below to learn how our partner sites have improved efficiencies and TAT at their organizations.
